What Are Cartilage Lesions?
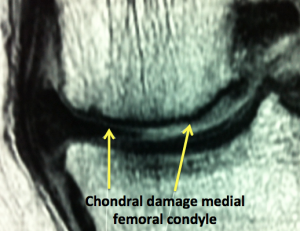
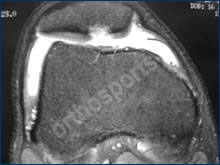
The reason our joints move smoothly is because they contain tissue specially designed to glide on itself. This shiny white lining is called chondral cartilage. Chondral cartilage is also known as articular or hyaline cartilage and it allows friction free gliding of the opposing joint surfaces (which permits smooth, pain free motion of the joint).
Sometimes people refer to the meniscus in the knee as the cartilage of the knee but this is not actually correct and becomes a bit confusing. The meniscus is the main shock absorber of the knee joint and is made up of type 1 collagen in a complex pattern designed to protect the joint lining or chondral cartilage. Articular cartilage is normally extremely smooth and is able to absorb some shock and continue to run smoothly despite the extreme loads placed upon it. Unfortunately when the chondral cartilage is damaged it is not able to repair itself. When the damage is severe the underlying bone is exposed and the loss of the friction free surface results in pain, catching and swelling (the definition of arthritis is damage to the joint lining cartilage). Unfortunately once the damage starts it can never be stopped but the rate at which the damage progresses can be altered by modifying your activities to reduce impact loading on the joint.
Many techniques have been used to try to repair the articular cartilage. The technology in this area is advancing all the time and the two most promising techniques currently are MACI (matrix-induced chondrocyte implantation) and stem cell injections. MACI has been developing over the last ten years and is currently a viable alternative for certain patients with articular cartilage lesions. Stem cell injections are still experimental at this stage and are very expensive. We hope that this will become a useful treatment tool in the future.



Who Is Suitable For A Chondrocyte Transfer Procedure?
If arthritis has already set into the knee then articular cartilage grafting will not work. It is rarely necessary under the age of 15 and does not work very well over the age of 50. The following criteria need to be met to make cartilage grafting successful:
- The pain must be located in a specific part of the knee (rather than the whole knee hurting).
- The damaged cartilage must be well localised (located in one area rather than all over the knee).
- The knee must be stable (no significant ligament damage).
- There must be normal limb alignment (not too knock kneed or bow legged).
- You must be well motivated for rehabilitation as a lot of physiotherapy is required.
- You must not have inflammatory arthritis (No rheumatoid arthritis, gout etc).
- Your body weight must be less than 1.5 times ideal body weight (Not very overweight).

What Is Done?
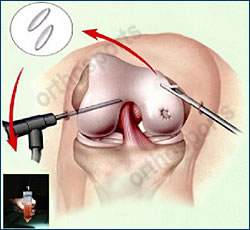
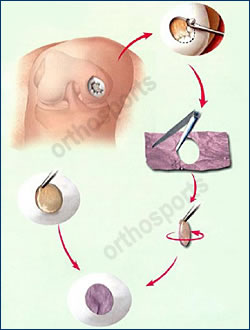
Treatment of articular cartilage injuries always requires at least two operations. The first is an arthroscopy to diagnose the injury and to harvest some of the normal cartilage cells from your knee. A piece of normal cartilage about the size of a tic tac is taken from an area in which it is not needed. This is then sent to a laboratory where it is cultured (a small number of cartilage cells are grown and multiplied into a large number of cells). These cells are grown in a membrane which is stored for later use. At the second operation (which is often anything from 6 weeks to 6 months later) the knee joint is opened (not arthroscopic or keyhole surgery like the first operation) and the damaged area is tidied up (debrided) to create a smooth base and smooth edges into which the new cells can be placed. The special membrane (much like a piece of felt), which contains the chondral cells which were grown in the laboratory, are “glued” into place to fill the defect as seen in the diagrams above and below.
If you have any mal-alignment (the leg is bowed) this may need to be corrected with a high tibial osteotomy at the time of the operation to take the pressure off the damaged area.
Most people only stay in hospital for one or two nights. You are seen by a physiotherapist who will teach you exercises which must be performed 3-4 times per day. The specific exercises will vary depending on the location of your cartilage defect. Most people commence immediate motion of the knee and are allowed to put some weight through the leg (partial weight bearing) for 6 weeks and then increase to full weight bearing by 12 weeks. This again depends on the location of the articular cartilage injury.
The cartilage takes 12 – 18 months to mature fully so patients typically do not return to load bearing exercises before the 12 month mark. Non loading bearing exercises such as swimming and cycling are started much earlier.
This operation is usually done to relieve pain and swelling on a day to day basis rather than to return people to high level sport.
You may need to wear a knee brace to limit the amount you can bend your knee after the operation. A graduated exercise programme will be given to you but will vary from patient to patient. A general guide for postoperative care is listed below.
This operation is not designed to get you back to sport. It is to prevent the onset and progression of arthritis in your knee. Returning to sporting activities should be considered a bonus (if it is possible) rather than an expected outcome of the surgery. As a general rule it is not possible to return to sports involving running and twisting for 12 months.
The time taken to return to work will depend on what work you do. If you sit at a desk all day and can be driven to and from work then you will probably be able to return to work on crutches at 10-14 days after the chondral grafting operation. Recovery from a high tibial osteotomy is slower and usually associated with more pain. Physical jobs, particularly those involving walking and lifting, may take 6 months or longer.
Rehabilitation varies greatly between patients as it depends on the size and site of the lesion. No two knees are exactly the same. The amount of weight you will allowed to take on the leg and the amount of bend you are allowed will depend on the location of the chondral lesion seen at surgery. If the damaged area in in a part of the knee which does not take load when you are walking then the whole process can be accelerated.
Week 1
- Allow wound healing
- Weight bearing – nil
- Motion – nil or slight flexion except if on CPM machine
- Brace – locked as appropriate
- Ambulation – crutches
- Physio – rest
Week 2-6
- Weight bearing – none to partial
- Motion – passive up to 90 degrees
- Brace – limited flexion
- Ambulation – crutches usually non weight bearing
- Physio – reduce swelling, closed chain, isometric quads, gentle cycling, walking or treading water in a pool
Week 6-12
- Weight bearing – progress to full
- Motion – progress to full
- Brace – discard
- Ambulation – wean off crutches
- Physio – open chain, proprioceptive exercises, resisted cycling, swimming avoiding breaststroke
Week 12-52
- Gradual increase in all exercises to strengthen quads and hamstring muscles, jogging at 6 months, sport by 12 months
This procedure has good results for localised articular cartilage lesions. Without treatment a lot of these lesions progress to arthritis. It does involve a lot of rehabilitation and commitment to physiotherapy but once this is over the majority of patients are happy with their outcome.